Abstract
Introduction We conducted a meta-analysis in order to get a better understanding of which asparaginase formulation instigated thrombosis more intensely when treated. We also interested in the knowledge of whether the control or the intervention group (LMWH) works better as prophylaxis in either ASP formulation.
Methods
Searches for relevant articles within adult enrolled studies (abstracts, RCT, cohort / control, case series), from data bases such as PubMed, Medline. They may be single arm, with or without control, or head-to-head comparative studies.
Review studies in AALL adult patients treated with either NEA or PEG regimens between 2006 and 2021, involving the use of these agents in any or all phases of chemotherapy and document their respective VTE incidences. Review of study designs (prospective, retrospective, interventional, RCT, comparative studies etc.) with VTE incidence reported as primary or secondary objective.
Ph positivity AALL are excluded.
Thrombosis incidences from the studies are identified and documented. We compare the VTE incidences of published studies using either the NEA or the PEG formulation, with or without VTE prophylaxis for AALL treatment. Patients treated in all phases of the AALL protocol are eligible for inclusion analysis. Studies using LMWH as prophylaxis intervention either as a single arm or in comparison with control are included.
Categorize published studies into two main groups of studies utilized either NEA or PEG as integral part of the AALL treatment regimens.
Results: We have reviewed 144 articles; 10 articles met the inclusion criteria and were used for final data analysis. Four of 10 studies were interventional compared with control. Six of 10 studies were single arm in nature.
Incidences of VTE
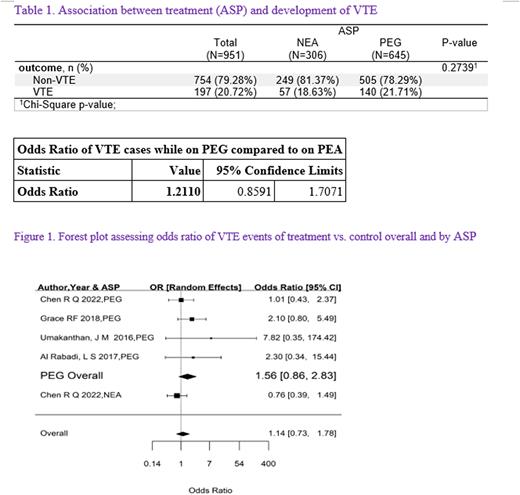
Table 1 illustrated association between treatments containing PEG or NEA and the development of VTE. A total of 951 patients were considered in the analysis. 306 patients were treated with NEA while 645 were receiving PEG in the studies. A total of 197 (20.72%) patients developed VTE, of which 57 (18.63%) were from the NEA recipients and 140 (21.71%) were treated with PEG. There was higher proportion of VTE incidences calculated in the PEG population compared to NEA recipients, but not significantly different (p= 0.2739).
Odds ratio was 1.2110 (95% CI 0.86-1.71)
Prophylaxis intervention vs. control
A Forest plot was used to assess the odds ratio of VTE incidences in prophylaxis intervention group vs. control and by either ASPs. While prophylaxis with LMWH appeared to have a larger impact (i.e. favored the intervention) on VTE prevention in PEG recipients, the lower limit of the OR did crossed the line of no effect (1.56 (0.86, 2.83)). On the other hand, there was only one study (Chen R. 2022) involving NEA that was clearly in favor of using the control (i.e. no prophylaxis) (Fig.1).
In a subgroup analysis, we compared VTE incidences between PEG and NEA studies (Al Rabati et al., Umakanthan et al., Grace et al., and Chen et al.) using intervention vs. control, we found the following. The total number of PEG patients enrolled is 175 and of which 60 (34.29%) developed VTE, whereas the total number of NEA recipients enrolled was 214 and of which 45 (21.03%) developed VTE (p=0.0034 ). None of the studies reported major bleeding using LMWH as thromboprophylaxis.
Discussion/Conclusion We believe our meta-analysis is the first attempt used to determine differences between ASP formulations on thrombosis. While the proportion of patients treated with PEG has higher incident rate for VTE than the NEA recipients, the difference between the ASPs in the development of VTE in AALL treated patients is small (p= 0.2739). Furthermore, the benefit with the use of prophylaxis in PEG recipients is present but diminished as demonstrated here [OR (1.14, 0.73, 1.78)]. In our subgroup analysis, the difference in terms of VTE risk is significantly higher among PEG recipients. The number of interventional /control studies and the sample size accrued involving ASP formulations in general, for the prevention of VTE are few and far in between. However, more studies and larger sample size are needed to clearly define its niche in AALL in future studies. Having that said, a small number of published studies have demonstrated value with the use of LMWH as VTE prophylaxis. Newer agents such as the direct oral anticoagulants independent of antithrombin III presence, may provide a different level of thrombosis prevention.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal